Gastrointestinal Procedures
Colonoscopy
What is Colonoscopy?
Colonoscopy
is a procedure used to see inside of the colon and rectum. Colonoscopy detects inflamed tissues, ulcers, and abnormal growths. This procedure looks for early signs of colorectal cancer and helps doctors diagnose unexplained changes in bowel habits, abdominal pain, bleeding and weight loss.
How to Prepare for Colonoscopy
The doctor usually provides written instructions about how to prepare for colonoscopy. The process is called a bowel prep. Generally, all solids must be emptied from the gastrointestinal tract by following a clear liquid diet for 1 to 3 days before the procedure. Patients should not drink beverages containing red or purple dye. Acceptable liquids include:
- fat-free bouillon or broth
- strained fruit juice
- water
- plain coffee
- plain tea
- sports drinks, such as Gatorade
- gelatin
A laxative or an enema may be required the night before colonoscopy. A laxative is medicine that loosens stool and increases bowel movements. Laxatives are usually swallowed in pill form or as a powder dissolved in water. An enema is performed by flushing water, or sometimes a mild soap solution, into the anus using a special wash bottle.
Patients should inform the doctor of all medical conditions and any medications, vitamins, or supplements taken regularly, including:
- aspirin
- arthritis medications
- blood thinners
- diabetes medications
- vitamins that contain iron
Driving is not permitted for 24 hours after colonoscopy to allow the sedative time to wear off. Before the appointment, patients should make plans for a ride home.
Poor Prep Disadvantages
- Increased procedural time
- Decreased diagnostic yield
- Increased complication rate
- Doctors often can't see potentially dangerous pre-cancerous lesions
- Repeat colonoscopy
Gastrointestinal Procedures
Colonoscopy
What is Colonoscopy?
Colonoscopy
is a procedure used to see inside of the colon and rectum. Colonoscopy detects inflamed tissues, ulcers, and abnormal growths. This procedure looks for early signs of colorectal cancer and helps doctors diagnose unexplained changes in bowel habits, abdominal pain, bleeding and weight loss.
How to Prepare for Colonoscopy
The doctor usually provides written instructions about how to prepare for colonoscopy. The process is called a bowel prep. Generally, all solids must be emptied from the gastrointestinal tract by following a clear liquid diet for 1 to 3 days before the procedure. Patients should not drink beverages containing red or purple dye. Acceptable liquids include:
- fat-free bouillon or broth
- strained fruit juice
- water
- plain coffee
- plain tea
- sports drinks, such as Gatorade
- gelatin
A laxative or an enema may be required the night before colonoscopy. A laxative is medicine that loosens stool and increases bowel movements. Laxatives are usually swallowed in pill form or as a powder dissolved in water. An enema is performed by flushing water, or sometimes a mild soap solution, into the anus using a special wash bottle.
Patients should inform the doctor of all medical conditions and any medications, vitamins, or supplements taken regularly, including:
- aspirin
- arthritis medications
- blood thinners
- diabetes medications
- vitamins that contain iron
Driving is not permitted for 24 hours after colonoscopy to allow the sedative time to wear off. Before the appointment, patients should make plans for a ride home.
Poor Prep Disadvantages
- Increased procedural time
- Decreased diagnostic yield
- Increased complication rate
- Doctors often can't see potentially dangerous pre-cancerous lesions
- Repeat colonoscopy
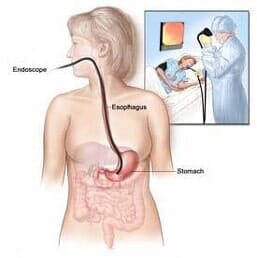
Endoscopy (EGD)
What is Upper Gastrointestinal (GI) Endoscopy?
Upper GI endoscopy is a procedure that uses a lighted, flexible endoscope to see inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum—the first part of the small intestine.
How to Prepare for Upper GI Endoscopy
The upper GI tract must be empty before upper GI endoscopy. Generally, no eating or drinking is allowed for 8 hours before the procedure. Smoking and chewing gum are also prohibited during this time.
Patients should tell their doctor about all health conditions they have—especially heart and lung problems, diabetes, and allergies— and all medications they are taking. Patients may be asked to temporarily stop taking medications that affect blood clotting or interact with sedatives, which are often given during upper GI endoscopy.
Medications and vitamins that may be restricted before and after upper GI endoscopy include:
- nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen (Advil), and naproxen (Aleve)
- blood thinners
- blood pressure medications
- diabetes medications
- antidepressants
- dietary supplements
Driving is not permitted for 12 to 24 hours after upper GI endoscopy to allow sedatives time to completely wear off. Before the appointment, patients should make plans for a ride home.
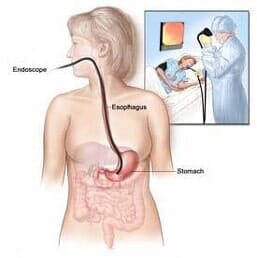
Endoscopy (EGD)
What is Upper Gastrointestinal (GI) Endoscopy?
Upper GI endoscopy is a procedure that uses a lighted, flexible endoscope to see inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum—the first part of the small intestine.
How to Prepare for Upper GI Endoscopy
The upper GI tract must be empty before upper GI endoscopy. Generally, no eating or drinking is allowed for 8 hours before the procedure. Smoking and chewing gum are also prohibited during this time.
Patients should tell their doctor about all health conditions they have—especially heart and lung problems, diabetes, and allergies— and all medications they are taking. Patients may be asked to temporarily stop taking medications that affect blood clotting or interact with sedatives, which are often given during upper GI endoscopy.
Medications and vitamins that may be restricted before and after upper GI endoscopy include:
- nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen (Advil), and naproxen (Aleve)
- blood thinners
- blood pressure medications
- diabetes medications
- antidepressants
- dietary supplements
Driving is not permitted for 12 to 24 hours after upper GI endoscopy to allow sedatives time to completely wear off. Before the appointment, patients should make plans for a ride home.
Points to Remember
- Upper gastrointestinal (GI) endoscopy is a procedure that uses a lighted, flexible endoscope to see inside the upper GI tract.
- To prepare for upper GI endoscopy, no eating or drinking is allowed for 4 to 8 hours before the procedure. Smoking and chewing gum are also prohibited.
- Patients should tell their doctor about all health conditions they have and all medications they are taking.
- Driving is not permitted for 12 to 24 hours after upper GI endoscopy to allow the sedative time to wear off. Before the appointment, patients should make plans for a ride home.
- Before upper GI endoscopy, the patient will receive a local anesthetic to numb the throat.
- An intravenous (IV) needle is placed in a vein in the arm if a sedative will be given.
- During upper GI endoscopy, an endoscope is carefully fed into the upper GI tract and images are transmitted to a video monitor.
- Special tools that slide through the endoscope allow the doctor to perform biopsies, stop bleeding, and remove abnormal growths.
- After upper GI endoscopy, patients may feel bloated or nauseated and may also have a sore throat.
- Unless otherwise directed, patients may immediately resume their normal diet and medications.
- Possible risks of an upper GI endoscopy include abnormal reaction to sedatives, bleeding from biopsy, and accidental puncture of the upper GI tract.
How To Prepare:
Preparation Sheet
Acid Reflux
Acid Reflux
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Endoscopic retrograde cholangiopancreatography is a procedure that combines upper gastrointestinal (GI) endoscopy and x rays to treat problems of the bile and pancreatic ducts. ERCP is also used to diagnose problems, but the availability of non-invasive tests such as magnetic resonance cholangiography has allowed ERCP to be used primarily for cases in which it is expected that treatment will be delivered during the procedure.
Wireless Capsule Endoscopy
What is Capsule Endoscopy?
Capsule endoscopy is also referred to as a wireless endoscopy. This procedure involves swallowing a video capsule to take photographs of the inside of the esophagus, stomach, and small intestine.
Why is Capsule Endoscopy done?
Capsule Endoscopy helps the doctor to evaluate the small intestine. This part of bowel cannot be reached by traditional upper endoscopy or by colonoscopy. The most common reason for doing capsule endoscopy is to search for a cause of bleeding from the small intestine. It may also be useful for detecting polyps, occult inflammatory bowel disease (Crohn's disease), ulcers, and tumors.
Points to Remember
- Upper gastrointestinal (GI) endoscopy is a procedure that uses a lighted, flexible endoscope to see inside the upper GI tract.
- To prepare for upper GI endoscopy, no eating or drinking is allowed for 4 to 8 hours before the procedure. Smoking and chewing gum are also prohibited.
- Patients should tell their doctor about all health conditions they have and all medications they are taking.
- Driving is not permitted for 12 to 24 hours after upper GI endoscopy to allow the sedative time to wear off. Before the appointment, patients should make plans for a ride home.
- Before upper GI endoscopy, the patient will receive a local anesthetic to numb the throat.
- An intravenous (IV) needle is placed in a vein in the arm if a sedative will be given.
- During upper GI endoscopy, an endoscope is carefully fed into the upper GI tract and images are transmitted to a video monitor.
- Special tools that slide through the endoscope allow the doctor to perform biopsies, stop bleeding, and remove abnormal growths.
- After upper GI endoscopy, patients may feel bloated or nauseated and may also have a sore throat.
- Unless otherwise directed, patients may immediately resume their normal diet and medications.
- Possible risks of an upper GI endoscopy include abnormal reaction to sedatives, bleeding from biopsy, and accidental puncture of the upper GI tract.
How To Prepare:
Preparation Sheet
Acid Reflux
Acid Reflux
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Endoscopic retrograde cholangiopancreatography is a procedure that combines upper gastrointestinal (GI) endoscopy and x rays to treat problems of the bile and pancreatic ducts. ERCP is also used to diagnose problems, but the availability of non-invasive tests such as magnetic resonance cholangiography has allowed ERCP to be used primarily for cases in which it is expected that treatment will be delivered during the procedure.
Wireless Capsule Endoscopy
What is Capsule Endoscopy?
Capsule endoscopy is also referred to as a wireless endoscopy. This procedure involves swallowing a video capsule to take photographs of the inside of the esophagus, stomach, and small intestine.
Why is Capsule Endoscopy done?
Capsule Endoscopy helps the doctor to evaluate the small intestine. This part of bowel cannot be reached by traditional upper endoscopy or by colonoscopy. The most common reason for doing capsule endoscopy is to search for a cause of bleeding from the small intestine. It may also be useful for detecting polyps, occult inflammatory bowel disease (Crohn's disease), ulcers, and tumors.
